Dr. Caroline Cupit
This blog sits at the intersection of my professional and personal experiences. I am a social scientist at University of Leicester, and I use ethnographic and qualitative interview methods to study the social organisation of healthcare, and to support quality improvement. I also have previous experience in hospice care.
This blog is about my recent personal experience of a COVID19-related end-of-life initiative that targeted an elderly relative. Such initiatives, involving the documentation of preferences in case of ‘serious illness’, are being increasingly targeted at older people—and especially with the advent of COVID-19. Although the intention is to ensure better care at the end-of-life, I hope my personal experience can shine a light on important questions relating to why they are needed, and how they are being implemented in practice. Many of us will be affected.
Recently, my elderly relative ‘Emma’ (not her real name) received a letter from her general practice surgery. The letter refers to a “government directive” for surgeries to undertake Treatment Escalation Plans for patients who are “currently on the shielded list because they are considered to be frail or highly vulnerable for severe coronavirus infection”.

Treatment Escalation Plans are a variation on Advance Care Plans, which are increasingly being employed in the care of people who are anticipated to be towards the end of their lives. They are supposed to facilitate patient autonomy and improve their quality of life, by ensuring that preferences (such as avoiding aggressive medical care) are recorded. However, the challenges of sensitively compiling these plans and the importance of personalised conversations are well-recognised.[1,2]
The letter that Emma received is more sensitively written than other examples I have seen, but it nonetheless arrived as a troublesome intrusion. It was pre-empted by a phone call from a rather officious practice nurse who tried to book an appointment for a phone conversation—which Emma stalled. Instead, Emma vaguely mentioned to me that the practice wanted her to put her affairs in order and what did I think about that?!
Emma found it difficult to articulate her reaction to the letter—neither her obvious repulsion and anxiety, nor her preferences in the case of serious complications with COVID19. Eventually, she articulated something along the lines of “the practice should know already” and “my family will make the right decision at the time”. She was upset to be forced into considering the issues raised in an abstract fashion. The letter jarred with her perception that the doctor should know her, and likewise family would understand her general preferences and would be able to sensibly apply them when needed.
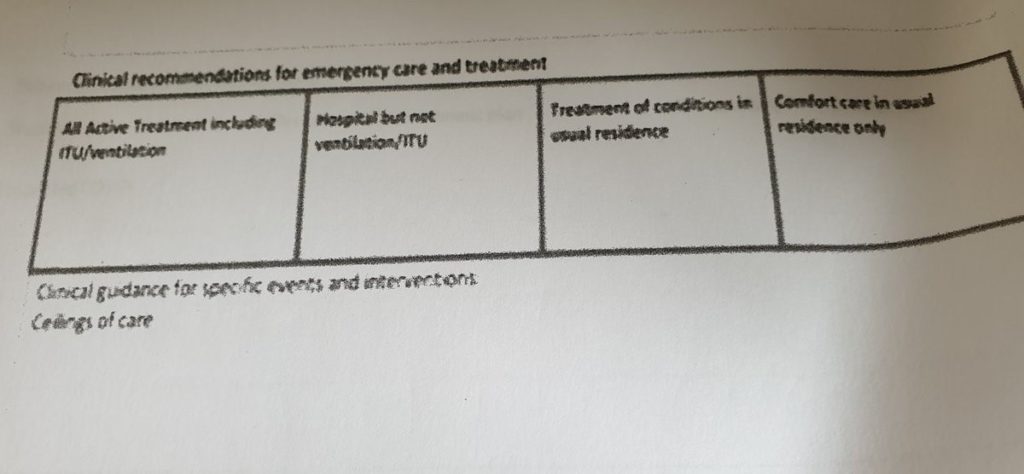
Dorothy Smith’s “sociology for people” [3-5] has been a useful ‘thinking tool’ of my professional work, and I apply it here to explore the uncomfortable position in which Emma and her family find themselves. Smith’s sociological framework, also known as “institutional ethnography”, begins by exploring common everyday interactions which have been shaped by institutional forces. It pays particular attention to how these everyday experiences are coordinated by texts and documents within healthcare and other institutions. I have previously found this approach useful to explore negative patient experiences of disease prevention in general practice—from the ‘ground’ and ‘up’ into remote institutional relations.[6,7] The Treatment Escalation Plan can be understood as a standardised ‘text’ that encodes local, contextualised knowledge into official knowledge and is used to coordinate the activities of clinicians, patients and families. Using this framework to explore Emma’s perspective, the difficulty caused by the letter can be understood as a clash between two different ‘forms of knowledge’. The first is abstract (official) knowledge of Emma that will be documented on the Treatment Escalation Plan form. The second is a personal (local and contextualised) knowledge of Emma. To complete the form, Emma and her family will have to somehow squeeze rich personal knowledge of Emma into the form’s predetermined categories. The boxes (e.g. ‘comfort care in usual residence only’) invite Emma to tick (or not). These instructions will then be applied to an uncertain future event.
Many different peoples’ activities are interlinked and coordinated by the Treatment Escalation Plan. The blank form and related polices have already been involved in the everyday work of clinicians and administrators at the surgical practice. Emma engages in the emotion work of extensive worry about how to broach the topic with her family (some of whom she thinks will also find it stressful). Her family also then engages in practical activity—deciding whether or not to draft a written response to the practice. If filled out, the form will (presumably) then be employed by a clinician whose work it is to treat Emma in the future. Treatment Escalation Plans are also a result of, and shape, broader policy discourse about appropriate end of life care, involving hundreds if not thousands of stakeholders.
Smith’s “sociology of the people” highlights the lived experiences and difficulties of individuals who are subjects of institutional activities, rather than only focusing on the ideals of care these types of practices are meant to facilitate. It can also bring visibility to the ways in which institutional practices contradict policy intentions, as made clear by Emma’s story, and therefore how systems may be improved. I hope that, for the benefit of patients like Emma, someone will investigate Treatment Escalation Plans and their institutional coordination.
Caroline Cupit is a Research Associate with the SAPPHIRE group at University of Leicester (Social Science APPlied to Healthcare Improvement Research). She is currently supported by a Mildred Blaxter Post-Doctoral Fellowship from the Foundation for the Sociology of Health and Illness and is exploring a growing movement to promote low-carbohydrate diets in healthcare. Her doctoral work was an ethnographic study of cardiovascular disease prevention in general practice. She has a particular interest in the use of ethnographic and qualitative interview methods (especially institutional ethnography) to support quality improvement, and to study the social organisation of healthcare settings.
[1] Mullick A, Martin J, Sallnow L. An introduction to advance care planning in practice. BMJ 2013;347:f6064–f6064. https://doi.org/10.1136/bmj.f6064.
[2] Zwakman M, Jabbarian LJ, van Delden JJM, van der Heide A, Korfage IJ, Pollock K, et al. Advance care planning: A systematic review about experiences of patients with a life-threatening or life-limiting illness. Palliat Med 2018:0269216318784474.
[3] Smith DE. Institutional Ethnography: A Sociology for People. Rowman Altamira; 2005.
[4] Smith DE. Institutional Ethnography as Practice. Rowman & Littlefield; 2006.
[5] Campbell M, Gregor FM. Mapping Social Relations: A Primer in Doing Institutional Ethnography. University of Toronto Press; 2002.
[6] Cupit C. An ethnographic study of cardiovascular disease prevention: the social organisation of measures, knowledge, interventions and tensions in English general practice. PhD Thesis. University of Leicester, 2018.
[7] Cupit C, Rankin J, Armstrong N, Martin GP. Overruling uncertainty about preventative medications: the social organisation of healthcare professionals’ knowledge and practices. Sociol Health Illn 2019;n/a. https://doi.org/10.1111/1467-9566.12998.

