Several years ago, I started hearing about a new kind of community-based care role. Some called themselves ‘end-of-life doula’; others identified themselves as a ‘death doula’ or a ‘death midwife’. These terms describe people (primarily women) who provide a wide range of social, emotional, practical, and spiritual supports for people nearing the end of life, including those close to them. This new role is often connected to the ‘doula’ role popularized by the natural birth movement in the 1970s, when the term was first used to describe lay-trained women providing nonmedical assistance during and after pregnancy.
As a medical anthropologist interested in end-of-life care, I became increasingly curious about these practitioners, what kinds of care work they do, and why they suddenly seemed to be so popular. The emergence of end-of-life doulas may evidence an important new development in our collective norms, desires, and concerns about the end of life and end-of-life care. However, I found there was very little known about them outside of a few newspaper articles and a handful of journal articles stating the need for further research.
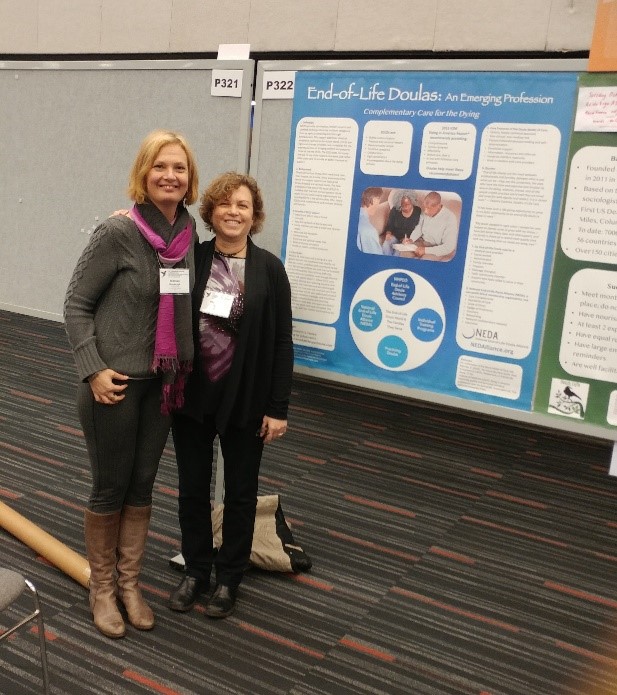
It therefore felt particularly serendipitous when I met Merilynne Rush in the last hours of the International Congress on Palliative Care in Montreal, in the fall of 2018. As an end-of-life doula educator and trainer in the United States, Merilynne was attending the conference to raise awareness about end-of-life doulas and seek research collaborators. You can out more about her work here. By the end of our initial conversation, we had firmly established our mutual interest in building an international research relationship.
Over the next year we co-designed and conducted a series of 22 in-depth interviews with key stakeholders and early innovators in community-based end-of-life care in Australia, Canada, the United States, and the United Kingdom. Our goal was to learn about the history, development, practices, and future potential of end-of-life doulas within these four countries where the end-of-life doula ‘movement’ is most active.
We are pleased to announce the first results of this collaboration, “Describing the end-of-life doula role and practices of care: perspectives from four countries” is now available as an open access article through Palliative Care & Social Practice.
Our findings evidence the grassroots history of this role, which is still developing and in flux. This was reflected in the enormous diversity of participants’ perspectives and experiences, and how they identified and described the end-of-life doula role and its practices. We found that, along with the name of this new role continuing to be a source of difference and debate, practitioners also did not adhere to a mutually agreed-upon set of practice standards. While these differences were seen as a significant challenge to professional development, and to public recognition and trust in the role, at the same time many participants articulated this diversity as desirable and necessary characteristic their work – in defining the benefits of the role operating outside of limiting bureaucratic health systems, in valuing the different types of practitioner knowledge and experience, and in honouring the unique relationship needs of each client and family. As summed up by one practitioner “It’s a bit woolly in a way but the wooliness is out of necessity”. We also found significant jurisdictional differences in health insurance coverage, hospice palliative care models, assisted dying legislation, and funeral industry regulations.
Collectively, the results of our research lead us to speculate that these tensions and within the end-of-life doula role, and regional differences, are potentially similar to the ‘growing pains’ experienced by other now-professionalized forms of caregiving – including hospice and palliative care. At the same time, we believe that this role may continue to develop alongside, but separate from, formal bureaucratic frameworks of professionalized care as a new hybrid community-entrepreneurial social movement.
If you’d like to learn more, you can listen to our recent End of Life Studies podcast episode.
We will be discussing our research further on January 22nd through the International Federation of Ageing’s Virtual Town Hall Series. You can find out more and register by clicking the button here:

Finally, below are a series of video shorts covering a range of different end-of-life doula topics, in conversation with Jennifer Mallmes, the Director of the Canadian End of Life Doula Association.
Who Identifies as an End of Life Doula?
Why are People Drawn to Becoming an End of Life Doula?
End of Life Doulas: The Relationship to Hospice and Palliative Care
Different Threads of End of Life Doula Philosophy and Practice
End of Life Doulas Becoming ‘Mainstream’
End of Life Doulas: Types of Knowledge
The Relevance of Research to End of Life Doulas


I wonder if this interesting collaboration could form the basis of a way to give back holistic End of Life care back to our communities. Perhaps using the death cafe model to promote active involvement in end of life support within family and community. The role of the “Death Doula” strikes me as a parallel to the role of the midwife, in French Sage-femme (wise woman), and this has role has been removed from the centre of the female community into a professional medicalised specialty. Perhaps the Death Doula may become over time another layer of professional help that may get in the way of lay people rediscovering their community support roles. In the “infancy” of this discipline perhaps a broad view could help retain and revitalilse community involvement. As a young man in a town of 3000 souls the two local joiners made the coffins and one organised the funeral with local clergy, my aunt, who died in 1960, was washed and dressed by her nieces and lay in her parlour for family and friends to visit. Similarly I watched with my cousins whose father died suddenly in 1967 as he lay in his coffin in the “best” room. There is a myth cultivated around death that bodies are somehow dirty and carriers of disease and therefore must be removed for the safety of the living. I have watched this change take place over the past 50 years to an expectation that professionals will do the “job” and community involvement has become diminished. Of course it has become even worse during the current pandemic when “safety” and infection control has further removed the family and community from the experience of dying and death and funeral customs. I kook forward to reading more of this research undertaken by yourself and Merilynne Rush.